Psoriasis is a chronic skin autoimmune skin condition though not fatal can be extremely irritating and traumatic. Although the disease is of a non-contagious nature, it can remain affecting a patient in cycles where there may be signs of remission only to resurface after a few weeks. The condition results in thickening and scaling of the skin surface where your skin may become dehydrated, dry, and flaky with constant itching. Psoriasis flare ups can severely impact mental well-being and affect one’s quality of life which is why understanding the disease, its causes, and how it can be treated is integral to its management.
What is Psoriasis?
Psoriasis is an autoimmune noncommunicable disease (NCD) for which there is no cure. The condition severely impacts the quality of life leading to joint deformations and disability putting people at risk of developing other serious clinical conditions such as cardiovascular disease and other NCDs.

In psoriasis, the immune system is triggered and activated into thinking harmful pathogens are attacking your system. The inflammatory response of your immune system then leads to rash, skin discoloration, joint swelling, and flaking of skin. In some cases, it can be mild but in others it can be extremely severe. The most common affected parts are the extremities such as ankles, knees, elbows, and the scalp beginning with typical reddening of the skin where patches soon start appearing. The biggest problem in the condition is the continued friction between extremities especially in over weight patients where mobility becomes painful.

Psoriasis also includes other comorbidities such as psoriatic arthritis (PsA) where the disease progresses to affect healthy joints and tissues resulting in inflammation and, over time, joint damage. It is estimated that around 30% of individuals with psoriasis eventually develop psoriatic arthritis.
Psoriasis Prevalence World Wide
According to the National Psoriasis Foundation, 125 million people suffer from the disease worldwide. In India, it affects 0.44-2.8 per cent of the population commonly affecting individuals in their third or fourth decade with males being affected two times more common than females1.
Causes of Psoriasis
The exact cause of psoriasis remains elusive, but researchers believe it results from a complex connection between genetic, weakened immunity and environmental factors. Environmental influences and unhygienic conditions can play a role in serious attacks of the skin condition. Moreover, infections, stress, and certain medications, can also increase psoriasis or trigger its onset in genetically susceptible individuals. Till date there has been no specific discovery on the root cause of psoriasis and the disease is still under extensive research with no documented age for people to develop it, but research has found how the disease usually attacks people post fifties.
- Genetic Factors: Psoriasis often runs in families, indicating a genetic component. Specific genetic markers associated with psoriasis susceptibility have been identified, linking the condition to variations in certain genes involved in the immune system.
- Immune System Dysfunction: Psoriasis is fundamentally an immune-mediated disorder. In a normal immune response, white blood cells (T cells) help protect the body against infection and disease. In individuals with psoriasis, however, these T cells become overactive, leading to an increased production of skin cells and the formation of plaques.
- Environmental Triggers: Certain environmental factors can act as triggers for psoriasis. These include infections (such as streptococcal throat infections), stress, smoking, and certain medications (like lithium, antimalarial drugs, and beta-blockers).
Possible Triggers
- Mental stress, anxiety, and tension which aggravate flareups
- Superficial skin injuries if infected can causes mild to severe psoriasis
- Streptococci infection like strep throat can cause skin rashes and psoriasis in youngsters
- Prolonged use of non-steroidal anti inflammation medication can worsen the condition.
- Sunlight is still debatable as a trigger or treatment in psoriasis.
- Alcohol and smoking are known triggers of most skin conditions.
- Cold weather can worsen psoriasis flares due to less sunlight and humidity, heated and drier indoor air. Warm weather can often improve it because of natural sunlight and higher humidity.
How Psoriasis Occurs and Different Types
Psoriasis is a condition resulting from the excessive activity of white blood cells or lymphocytes to produce inflammatory substances and chemicals which then attack skin cells making them grow too fast. It manifests in 5 variations of the disease, each presenting distinct symptoms and signs which include plaque, guttate , inverse, pustular, and erythrodermic psoriasis.
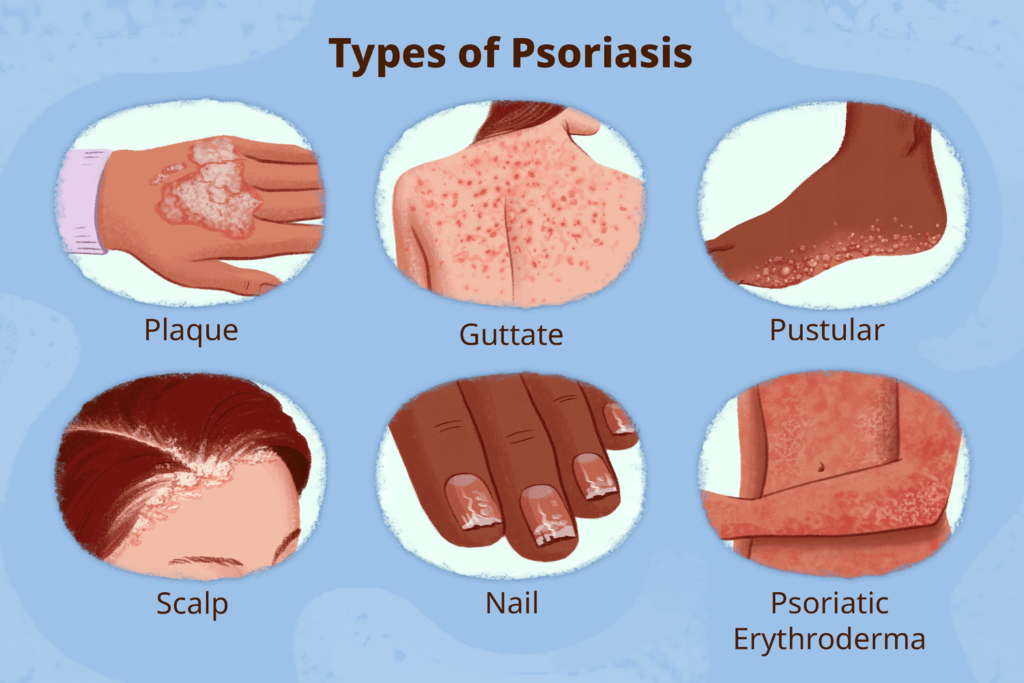
Plaque Psoriasis: This is the most prevalent form, characterized by raised, red patches covered with a silvery-white buildup of dead skin cells. These patches, known as plaques, can appear anywhere on the body but commonly affect the elbows, knees, scalp, and lower back.
Guttate Psoriasis: Typically triggered by a bacterial infection, guttate psoriasis appears as small, red or pinkish spots on the skin mainly on the arms and legs. It often occurs in children and young adults and may follow a streptococcal infection.
Inverse Psoriasis: Inverse psoriasis affects the skin folds, such as the underarms, groin, anal area and beneath the breasts. It appears as smooth, red lesions without the typical scaling seen in other forms of psoriasis.
Pustular Psoriasis: This form is characterized by the presence of pus-filled blisters on the skin. Pustular psoriasis can be localized to specific areas or widespread, and it may be accompanied by fever, chills, and other systemic symptoms.
Erythrodermic Psoriasis: Erythrodermic psoriasis is a severe and rare form that can cover the entire body with a red, peeling rash that continues to shed and flake. This type of psoriasis can be life-threatening and requires immediate medical attention.
Diagnosis and Risk Factors of Psoriasis
Diagnosis of psoriasis is not a complicated process as the disease is a visible condition of the skin. In stubborn conditions it would need a skin biopsy and X rays to determine the extent of the disease. Patients with prolonged and severe psoriasis are at risk of contracting related diseases such as the ones mentioned below.
Treatment
While there is no cure for psoriasis, various treatment options can help manage symptoms, reduce inflammation, and improve the quality of life for individuals with this condition. Treatment plans are often personalized based on the severity, the type, and the patient’s overall health with treatments including the use of moisturizers and skin creams. For scalp conditions, herbal and medical shampoos are used with conditioners for reducing the dryness of scalp. As psoriasis is caused by excessive dry skin, keeping skin permanently moist is necessary. In severe conditions, a combination of oral and external medication is necessary
Topical Treatments
These include creams, ointments, and lotions applied directly to the skin. Corticosteroids, vitamin D analogs, retinoids, and coal tar preparations are examples of topical treatments that can help alleviate symptoms.
- Cyclosporine: used effectively for psoriasis inflammation
- Calcipotriene: a topical cream prescribed in psoriasis and skin conditions
- Salicylic acid: helps in smoothening the rough skin condition and increases scale shedding to remove the inflamed skin.
- Otezla (Apremilast): the first advanced oral systemic treatment for Psoriasis in India.
- Coppellor (Ixekizumab) : The latest drug to be launched in India to treat moderate-to-severe plaque psoriasis
Phototherapy (Light Therapy)
Exposure to natural or artificial ultraviolet (UV) light can be beneficial in treating psoriasis. Phototherapy is often administered under medical supervision and can help slow down the rapid growth of skin cells.
Systemic Medications
For more severe cases of psoriasis, systemic medications may be prescribed. These can include oral or injected medications that work throughout the body to suppress the immune system and reduce inflammation.
Biologic Drugs
Biologics are a newer class of medications that target specific parts of the immune system involved in the development of psoriasis. These drugs are administered by injection and have shown significant success in managing moderate to severe psoriasis. The biologics currently in use for psoriasis in India are etanercept, infliximab and recently introduced itolizumab and secukinumab.
Lifestyle Changes
Making certain lifestyle modifications can also contribute to managing psoriasis symptoms. These include maintaining a healthy weight, avoiding smoking and excessive alcohol consumption, managing stress, and adopting a balanced diet rich in anti-inflammatory foods. Managing stress and anxiety can do much to reduce flare ups of psoriasis.
Time Tested Home Remedies for Skin Care and Psoriasis
- Aloe Vera: Aloe Vera creams like derma dew are widely used I skin conditions where aloevera contains popular skin rejuvenation and moisturizing properties
- Fish oil: Using fish oil on the affected areas can work wonders for psoriasis.
- Oatmeal. Oatmeal soaks are good for soothing psoriasis
- Dead Sea salts and Epsom salts: Make a solution with Epsom salts and lukewarm water to soothe and reduce irritation.
- Neem: Bathing in Neem water or using neem oil is beneficial for soothing skin problems and relieving itching.
Psoriasis is a chronic and multifaceted skin condition that requires a comprehensive understanding of its causes, symptoms, signs, and treatment options. While there is no cure, advancements in medical research and treatment modalities have significantly improved the quality of life for individuals living with psoriasis. Seeking prompt medical attention, adopting a personalized treatment plan, and making positive lifestyle changes can help individuals effectively manage their psoriasis and lead fulfilling lives. If you suspect you have psoriasis or are experiencing skin-related concerns, consult with a healthcare professional for an accurate diagnosis and appropriate management plan tailored to your specific needs.