Coronary Artery Disease (CAD) is a prevalent cardiovascular condition that affects millions of people worldwide. According to a Lancet study, cardiovascular disease is the leading cause of death in India. Calling it a CVD epidemic, the study found how cardiovascular disease in India was mainly due to a higher risk burden, early age of onset, premature and higher fatalities. A study commemorating world heart day 2023 further stated how CVD is the world’s topmost killer with 80% of deaths premature. The most unfortunate aspect of CVD is how despite being treatable, detectable, and manageable in early stages, it is still the leading cause of fatality in the world.
CAD occurs when the blood vessels supplying the heart muscle (coronary arteries) become narrowed or blocked, leading to reduced blood flow to the heart. Referred to as also coronary heart disease or ischemic heart disease, the first sign of CAD can be a heart attack. Recognizing the signs and symptoms of CAD is crucial for early intervention, management, and prevention of further complications.
What is Coronary Artery Disease?
Coronary artery disease (CAD) refers to the narrowing or blockage of the coronary arteries, responsible for supplying oxygen-rich blood to the heart. This condition develops gradually as plaque, including cholesterol, accumulates within these arteries, restricting the flow of blood to the heart muscle which is a condition called myocardial ischemia or lack of blood flow to the heart. . Plaque consisting of cholesterol deposits, and other substances cause arteries to narrow over time developing into a condition called atherosclerosis, one of the main causes of CAD.
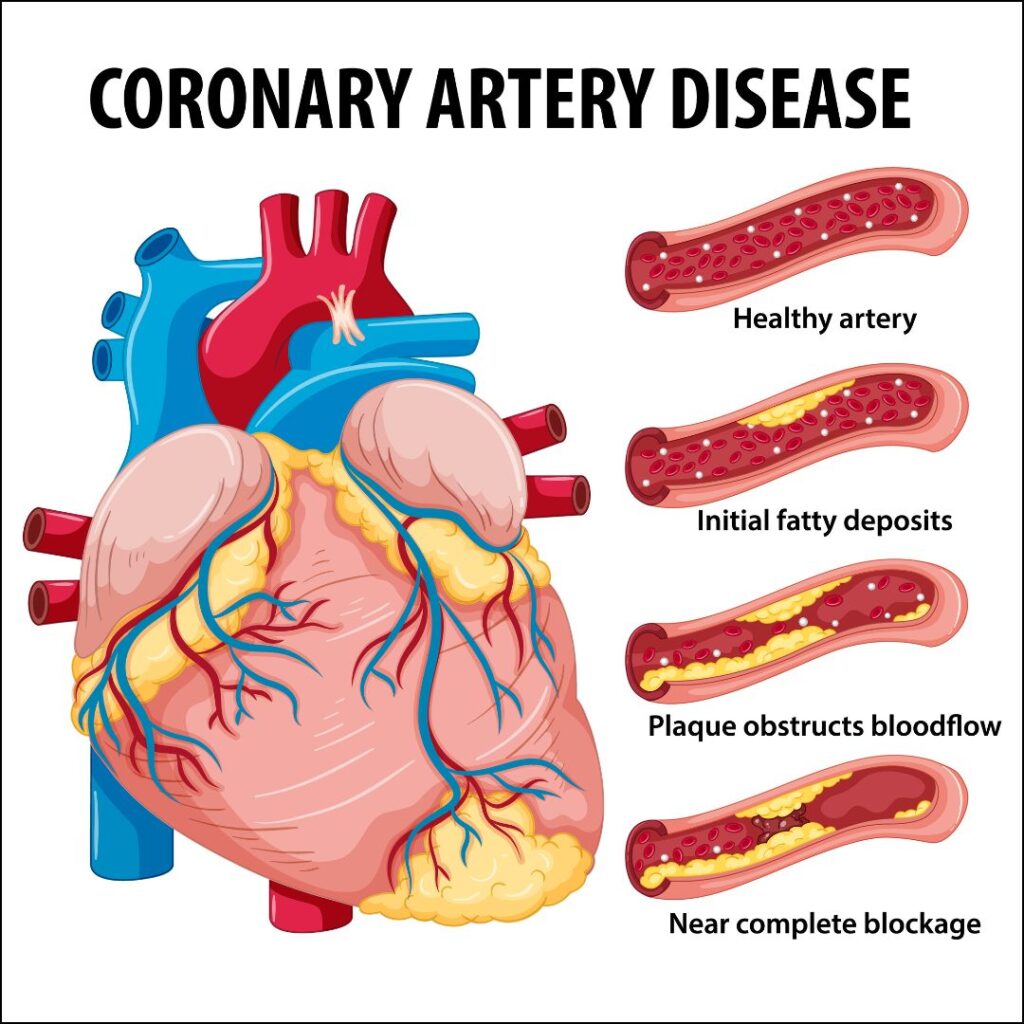
In CAD, symptoms may not be noticeable until the plaque triggers the formation of a blood clot, halting the flow of blood to the heart. When blood cannot efficiently reach the heart, it results in a heart attack. CAD can persist for years without any apparent symptoms until a heart attack occurs, earning it the moniker of a “silent killer.”
Types of CAD
Coronary artery disease manifests in two primary forms:
Stable Ischemic Heart Disease: This form is chronic in nature. Over the course of many years, your coronary arteries gradually narrow, leading to decreased oxygen-rich blood supply to the heart. While you may experience some symptoms, you can typically manage your condition on a day-to-day basis.
Acute Coronary Syndrome: This is the sudden and emergent form of the disease. In this scenario, the plaque within your coronary artery ruptures abruptly, forming a blood clot that obstructs blood flow to the heart. This sudden blockage triggers a heart attack. Signs and Symptoms:
Recognizing the signs and symptoms of CAD is crucial for early intervention and prevention of complications. Common manifestations include:
- Chest Pain (Angina): Stable angina is a common symptom of CAD and is often described as a discomfort or pressure in the chest. It may also be felt in the arms, neck, jaw, shoulder, or back. Angina typically occurs during physical exertion or emotional stress and is relieved by rest or nitroglycerin, a medication for angina.
- Shortness of Breath: CAD can lead to reduced blood flow to the heart muscle, affecting its ability to pump efficiently. This may result in shortness of breath, or Dyspnea especially during exertion or stress.
- Fatigue: Reduced blood flow to the heart can compromise its ability to meet the body’s oxygen demands, leading to fatigue and weakness.
- Sweating: Excessive sweating, particularly in conjunction with other symptoms, may be a sign of an impending heart issue. In most cases, a cold sweat is typical of CAD
- Pain: Pain or discomfort in the arms or shoulder
- Nausea and Dizziness: Insufficient blood flow to the heart can affect other organs, leading to symptoms such as nausea, lightheadedness, and dizziness.
It’s important to note that individuals may experience these symptoms differently, and some may not have any noticeable symptoms, a condition known as silent ischemia.
Causes of Coronary Artery Disease
Several factors contribute to the development of CAD. Understanding these risk factors is essential for both prevention and management. Key causes include:
- Atherosclerosis: The primary cause of CAD is atherosclerosis, a condition where fatty deposits (plaques) build up on the inner walls of the coronary arteries. Over time, these plaques can narrow the arteries, reducing blood flow to the heart. People with plaque build also acquire the risk of peripheral artery disease (PAD) and carotid artery disease.
- High Blood Pressure (Hypertension): Elevated blood pressure can strain the arteries and contribute to the development of atherosclerosis.
- High Cholesterol: Elevated levels of LDL cholesterol (“bad” cholesterol) and low levels of HDL ( Good cholesterol) can lead to the accumulation of plaques in the arteries.
- Smoking: Tobacco smoke contains chemicals that can damage blood vessels, promoting atherosclerosis.
- Diabetes: Individuals with diabetes are at an increased risk of developing CAD due to elevated blood sugar levels that can damage blood vessels.
- Family History: A family history of CAD increases the risk, suggesting a genetic predisposition.
- Age and Gender: Aging and being male are associated with an increased risk of CAD. However, post-menopausal women also face an elevated risk.
- Lack of Physical Activity: Sedentary lifestyles contribute to obesity and other risk factors for CAD.
- Lack of Sleep: Sleep loss might serve to elevate nocturnal catecholamine levels and contribute to cardiovascular disease.
- Disease: Autoimmune disease like lupus and rheumatoid arthritis, CKD, AIDS, Metabolic Syndrome, Endometriosis, and Preeclampsia.
- Birth Control: Use of Hormonal birth control pills.
Diagnosis of Coronary Artery Disease:
Diagnosing CAD involves a combination of clinical assessments, medical history, and diagnostic tests. Healthcare professionals may employ the following approaches:
Medical History and Physical Examination: The healthcare provider will inquire about the patient’s symptoms, medical history, and lifestyle factors. A physical examination may reveal signs such as high blood pressure or abnormal heart sounds.
Echocardiogram: Uses ultrasound (special sound wave) to create a picture of the heart.
Electrocardiogram (ECG or EKG): This test measures the electrical activity of the heart and can identify abnormal rhythms and signs of a previous heart attack.
Blood Tests: Cardiac blood tests can assess cholesterol levels, blood sugar, HRV, Troponin and other factors that contribute to CAD risk.
Stress Tests: These tests evaluate the heart’s response to physical stress, either through exercise or medication, to detect abnormalities in blood flow. Also called a TMT, you will most probably be made to walk on a treadmill while being monitored how well your heart is pumping.
Coronary Angiography: This invasive procedure involves injecting a contrast dye into the coronary arteries, allowing healthcare professionals to visualize blockages, and narrowing using X-rays.
Coronary Artery Calcium Scan: A computed tomography (CT) scan that looks in the coronary arteries for calcium buildup and plaque.
Cardiac CT or MRI: These imaging techniques provide detailed images of the heart and coronary arteries, helping to assess the extent of CAD
Cardiac Catheterization: This procedure involves examining the inner walls of your arteries to detect any blockages. A slender, flexible tube is inserted through an artery in the groin, arm, or neck to access the heart. Healthcare providers can assess blood pressure within the heart, evaluate the blood flow’s strength through the heart’s chambers, obtain blood samples directly from the heart, and administer dye into the coronary arteries for imaging purposes.
Complications in CAD
Coronary artery disease if not checked can eventually lead to further complications like
- Arrhythmias (abnormal heart rhythms).
- Cardiac arrest.
- Cardiogenic shock.
- Congestive Heart failure.
Treatment Options for Coronary Artery Disease
Once diagnosed, CAD management aims to alleviate symptoms, prevent complications, and improve overall heart health. Treatment options include:
Lifestyle Modifications: Adopting a heart-healthy lifestyle is fundamental in CAD management. This includes a balanced diet low in saturated and trans fats, regular exercise, smoking cessation, and maintaining a healthy weight.
Medications: Various medications may be prescribed to manage CAD, including antiplatelet drugs, statins to lower cholesterol, beta-blockers, and nitroglycerin for angina relief.
Angioplasty and Stenting: In cases of significant artery blockages, a procedure called angioplasty may be performed. This involves inflating a balloon within the narrowed artery to widen it, often accompanied by the placement of a stent to keep the artery open.
Coronary Artery Bypass Grafting (CABG): For more complex cases, CABG may be recommended. This surgical procedure involves using a healthy blood vessel (graft) from another part of the body to bypass the blocked or narrowed coronary artery.
Implantable Devices: In some instances, devices such as pacemakers or implantable cardioverter-defibrillators (ICDs) may be recommended to regulate heart rhythm.
Management Strategies for Coronary Artery Disease
Beyond medical interventions, ongoing management is crucial to control symptoms and prevent the progression of CAD. Key management strategies include
Monitoring Blood Pressure
Monitoring your blood pressure is a helpful way to understand if you’re experiencing high blood pressure which usually doesn’t have symptoms which is why it’s called the silent killer.
Regular Follow-up
Routine check-ups with healthcare professionals are essential to monitor the effectiveness of treatments and make necessary adjustments.
Timely Medication
It is vital to adhere to prescribed medications and follow the healthcare provider’s recommendations regarding dosage and frequency.
Cardiac Rehabilitation
Participating in a structured cardiac rehabilitation program can help individuals regain physical strength, improve cardiovascular fitness, and receive guidance on lifestyle modifications.
Stress management
Managing stress and addressing emotional well-being is integral to CAD management. Techniques such as mindfulness, relaxation exercises, and counseling may be beneficial.
Healthy Diet & Lifestyle
Eating a balanced nutritious diet and avoiding processed foods. Exercising daily such as walking helps. Avoid strenuous activity that places extra stress on your heart. Avoid smoking.
Read: 12 Foods that Clean Arteries and Reduce the Risk of Heart Disease
Coronary Artery Disease is a significant health concern that requires understanding, early detection, and effective management. Recognizing the signs and symptoms, understanding the causes, seeking timely diagnosis, and adopting a multifaceted approach to treatment and management are key components in the battle against CAD. By incorporating lifestyle changes, medications, and, when necessary, medical procedures, individuals can enhance their quality of life and reduce the risk of complications associated with this prevalent cardiovascular condition. Above all, you should always consult your doctor for personalized advice and guidance based on individual health needs.