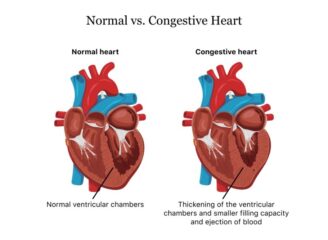
Congestive heart failure (CHF) is a complex condition of the heart affecting millions of people worldwide. Referred to as simply heart failure, CHF is a chronic and progressive condition where the heart struggles to pump blood enough to meet the body’s needs. Even though your heart continues to work, it’s weakened capacity to handle the amount of blood it should, leads to an accumulation of blood and fluid in areas like the lungs, legs, and feet.
CHF stands out among cardiovascular disorders due to its impact on the body’s circulatory system. It is almost like an overwhelmed delivery system that can’t distribute packages adequately, in this case, a failing heart which can’t pump blood effectively. This leads to a backlogs and potential complications.
Types of Heart Failure
While the overarching condition is termed congestive heart failure, there are subcategories based on its occurrence and affected region:
Left-sided heart failure: Impacts the heart’s left portion, impairing its ability to channel oxygen-rich blood to various parts of the body.
Right-sided heart failure affects the right side, leading to a blood backup as it enters the heart.
High-output heart failure: A rarer form where the heart must work harder due to other extenuating health conditions.
Symptoms of Congestive Heart Failure
Identifying congestive heart failure early can significantly affect management and quality of life. Common indicators include:
- Chest discomfort.
- Irregular heart rhythms.
- A consistent dry cough.
- Persistent breathlessness, even intensifying during sleep.
- Sudden weight fluctuations.
- Abdominal bloating or stiffness.
- Fatigue during mundane activities.
- Loss of appetite or accompanied nausea.
- Edema in the ankles, legs, or abdomen.
- Increased nocturnal urination.
It’s essential to understand that the severity and occurrence of these symptoms can vary. Some individuals might have sporadic mild symptoms, while others might experience them more intensely.
The grim reality is that congestive heart failure if left unchecked, can progressively intensify. As the condition advances, symptoms can manifest in new ways or grow in severity. However, early detection and intervention can play a pivotal role in managing its trajectory.
Understanding the Intricacies of Congestive Heart Failure
One of the most intricate systems in our bodies, the cardiovascular system, faces multiple challenges, including congestive heart failure. Delving deeper into the intricacies of this condition offers a comprehensive perspective on its causes, risks, complications, diagnostic methods, and stages.
Root Causes of Congestive Heart Failure
Several factors can contribute to the onset of congestive heart failure:
- Coronary Ailments: Coronary artery disease, often followed by heart attacks, stands out prominently.
- Cardiomyopathy: Either stemming from genetic sources or viral infections.
- Inherent Heart Conditions: Congenital heart diseases that have been present since birth.
- Chronic Conditions: Diabetes and high blood pressure (hypertension) can strain the heart over time.
- Organ Disorders: Kidney diseases, particular lung conditions, or disturbances in other organs.
- Lifestyle and Consumption: A higher body mass index (above 30), habitual tobacco use, and excessive alcohol consumption.
- Medicinal Side-effects: Certain cancer treatments like chemotherapy can impact heart functionality.
- Left-sided Heart Failure’s Domino Effect: Predominantly, a malfunctioning left ventricle can cause blood backup, eventually impacting the right ventricle.
Factors Heightening the Risk
Certain factors can predispose an individual to a higher risk of congestive heart failure:
- Individuals over the age of 65.
- Regular use of tobacco, cocaine, or alcohol.
- Sedentary lifestyles and diets rich in salt and fats.
- A lineage showcasing prevalent cases of heart failure.
- Personal history of high blood pressure, coronary artery diseases, or heart attacks.
Potential Complications Arising
Unchecked congestive heart failure might spawn severe health ramifications like- Abrupt cardiac arrests; Malfunctions in the heart valves; Accumulation of fluid within the lungs; Heartbeat irregularities; Escalation to pulmonary hypertension; Risk of undernourishment; Adverse effects on organs, leading to kidney or liver damages.
Diagnostic Approaches and Treatments
When your clinician diagnoses the potential symptoms, they will follow through on a systematic process for treatment. They begin by understanding the patient’s broader health condition, familial cardiac history, consumption habits, and any history related to chemotherapy or radiation. The next step is a clinical examination: An in-depth physical analysis to ascertain any overt signs of the ailment.
Progression Stages of Heart Failure
Congestive heart failure is progressive, methodically categorized into four distinctive stages:
Stage A
Labelled as a pre-heart failure, it signifies a looming risk due to factors such as hypertension, diabetes, coronary artery disease, history of specific disorders, or exposure to heart-damaging medications.
Stage B
Also, within the pre-heart failure realm, it indicates structural or functional anomalies in the left ventricle without the manifestation of heart failure symptoms.
Stage C
Individuals diagnosed at this stage either currently exhibit or have previously shown signs of heart failure.
Stage D
This final stage represents advanced heart failure symptoms with Reduced Ejection Fraction (HFrEF), unresponsive to standard treatments. A defining characteristic is the heart’s reduced capacity to pump blood, highlighting the dire nature of this phase.
Arming oneself with knowledge about congestive heart failure, from its causes to its stages, is essential for both prevention and management. Awareness allows for early detection, timely intervention, and a potentially improved quality of life for those affected.
Diagnostic Measures for Congestive Heart Failure
When faced with the potential onset of congestive heart failure, a series of diagnostic measures are employed to not only confirm the presence of the condition but also to pinpoint its severity and root cause:
- Blood Analysis
- Echocardiogram
- Cardiac Catheterization
- Stress Test
- Radiological Measures like chest X-rays
- Advanced Imaging such as Heart MRI (Magnetic Resonance Imaging) and Cardiac Computed Tomography.
- Electrocardiogram (EKG/ECG)
- MUGA Scan
- Genetic Exploration
A Multi-tiered Approach to Treating Congestive Heart Failure
Congestive heart failure is a significant medical condition, and its management and understanding are paramount. As a progressive ailment, it demands a versatile treatment plan tailored to its specific stage. While there’s no direct cure, the objective is to manage symptoms and impede its progression. The treatment protocols are stratified based on the stages of the disease.
Stage A: CHF Management
The initial approach emphasizes preventive measures and lifestyle modifications for those diagnosed with Stage A heart failure. Engaging in routine physical activity like daily walks can be beneficial. Furthermore, refraining from the use of tobacco is crucial.
Addressing underlying conditions like high blood pressure is fundamental. This might entail using medications, adhering to a low-salt diet, and maintaining an active lifestyle. High cholesterol levels should also be addressed. Abstaining from alcohol and strong drug usage is equally pivotal.
Stage B: CHF Intervention
The treatment plan for those in Stage B typically builds upon the Stage A measures. Key additions may include ACE inhibitors or angiotensin II receptor blockers, mainly if one’s ejection fraction (EF) is at or below 40%. Beta-blockers become crucial if there’s a history of a heart attack and the EF remains at or under 40%. An aldosterone antagonist might be considered post-heart attack or if the EF dips below 35%. Some cases might require surgical interventions, such as addressing coronary artery blockages, managing a previous heart attack’s repercussion, or treating valve diseases.
Stage C: CHF Approach
Individuals with Stage C HFrEF will likely have an extended treatment regimen encompassing strategies from Stages A and B. This might comprise beta-blockers, aldosterone antagonists, and Sodium-glucose transport 2 inhibitors (SGLT2i).
Heart rate regulation becomes vital if the rate exceeds 70 beats per minute, especially if symptoms persist. This can be achieved through specific medications. Maintaining optimal fluid balance may require diuretics. Dietary sodium restriction, daily weight monitoring, and possible fluid intake limits become essential. Advanced treatment modalities such as cardiac resynchronization therapy or implantable cardiac defibrillators might be explored. Even if symptoms decrease or stabilize, continued treatment remains indispensable to curtail the progression towards Stage D.
Stage D: CHF Solutions
Stage D patients undergo extensive treatments amalgamating interventions from previous stages. Furthermore, evaluations for advanced treatments, such as heart transplants, ventricular assist devices, or heart surgeries, are often considered. Continuous inotropic drug infusions and palliative or hospice care might also be explored to ensure the quality of life.
Medical Treatments for Stages C & D with Preserved EF
Those with preserved ejection fraction in Stages C and D require treatments from the earlier stages, coupled with medications that manage conditions potentially worsening heart failure. Regular diuretics usage can alleviate symptoms. It becomes pivotal to judiciously manage co-existing health issues like diabetes, kidney disorders, anemia, hypertension, thyroid anomalies, asthma, and chronic lung diseases. Some conditions can mimic heart failure, so communicating any new or intensified non-emergency symptoms to healthcare providers is crucial.
Potential Complications of Congestive Heart Failure
Interventions for congestive heart failure aren’t devoid of potential side effects or complications. These might include hypotension, kidney dysfunction, or infections associated with frequent hospital visits requiring IV access.
Prevention and Lifestyle Adaptations
To potentially stave off heart failure, one can adopt heart-healthy practices like maintaining optimal weight, consuming heart-friendly diets, regular exercise, effective stress management, abstaining from tobacco, alcohol, or recreational drugs, and meticulously managing existing health conditions.
Living Normally, even with Congestive Heart Failure
Although this may seem scary, with the right medical and self-care, many continue leading fulfilling lives despite the limitations imposed by heart failure. The prognosis largely hinges on the heart’s functional capacity, symptom severity, treatment responsiveness, and adherence to the medical regimen. Some studies suggest a reduced life expectancy, but individual circumstances play a significant role. It’s imperative to remain proactive about self-care: adhere to prescribed medications, maintain physical activity, adhere to dietary guidelines, and routinely update healthcare providers about any symptom changes. Preparing advanced directives can also provide clarity regarding medical wishes.
- Dietary Considerations: Salt and fluid intake might need restrictions. It’s essential to consult healthcare providers for tailored guidelines.
- Emergency Situations: Certain symptoms like intensified breathlessness or sudden weight fluctuations require immediate medical attention. In emergencies, immediate medical interventions can stabilize the condition.
- Questions for Healthcare Providers: Engaging in open dialogue with medical providers can be enlightening. Some pertinent questions might include understanding one’s heart failure stage, suitable treatments, exercise recommendations, and potential support groups.
In essence, while congestive heart failure is a long-term condition, one can lead a quality life with timely interventions, informed decisions, and active self-management.