Hypotension, or low blood pressure, is a condition that often goes undetected just like hypertension or high blood pressure. It is only when blood pressure levels drop drastically causing severe symptoms that detects a condition of low blood pressure. According to the standard consensus of blood pressure levels, low blood pressure is a reading below 90/60 mm Hg and can cause fainting spells and dizziness. However, not many people develop such symptoms unless blood pressure drops too low. Treating hypotension requires diagnosing the causes, medication, and lifestyle management.
What is Hypotension?
Your blood pressure involves two numbers:
Systolic (top number): The pressure your blood exerts on your arteries each time your heart beats.
Diastolic (bottom number): The pressure your blood exerts on your arteries when your heart rests between beats.
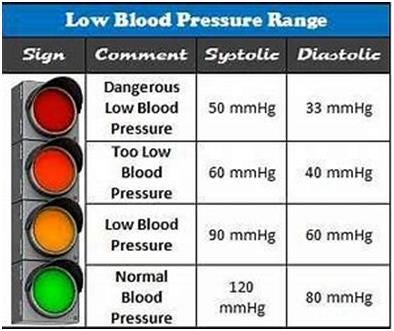
Hypotension is defined as abnormally low blood pressure, where the pressure of blood against the walls of the arteries is lower than normal. Typically, a blood pressure reading below 90/60 mmHg is considered hypotensive. However, it’s essential to recognize that what constitutes low blood pressure can vary depending on factors such as age, health status, and individual physiology. There are various types of low blood pressure.
Is Low Blood Pressure Common?
Hypotension is not as common as Hypertension or high blood pressure. Moreover, due to most cases being asymptomatic, very less data exists to know how many people it affects. However, low blood pressure tends to figure in people as they age and cross 50 with a higher prevalence in people over 70. Hypotension can also feature in younger people who are physically active, but without symptoms.
Types of Hypotension
Absolute hypotension: A resting BP measures below 90/60 millimeters of mercury (mm Hg).
Orthostatic hypotension: When blood pressure remains low for longer than three minutes after you stand up from a sitting position. Changing positions usually causes a change in BP, but these changes last just a few seconds. The drop must be 20 mm Hg or more for your systolic (top) pressure and 10 mm Hg or more for your diastolic (bottom) pressure. Orthostatic hypotension is also called postural hypotension due to changes in posture.
Causes of Low Blood Pressure
- Dehydration: Loss of fluids through vomiting, diarrhea, excessive sweating, or inadequate fluid intake can lead to a decrease in blood volume, resulting in low blood pressure.
- Low blood volume: Blood loss from injuries and illness can cause low blood pressure. Dehydration also contributes to low blood volume.
- Medications: Certain medications, such as diuretics, alpha blockers, beta blockers, and some antidepressants, can cause a drop in blood pressure as a side effect. Certain herbal supplements, vitamins or home remedies can also lower your blood pressure. This is why you should always consult healthcare provider before taking any medication or natural supplements.
- Heart and Lung Problems: Conditions like heart valve problems, irregular heart rhythms (arrhythmias), heart attack, pulmonary embolism (PE), congestive heart failure (weak heart muscles), collapsed lung, bradycardia (slow heart rate) or tachycardia (high heart rate) can impair the heart’s ability to pump blood effectively, leading to hypotension.
- Endocrine Disorders: Hormonal imbalances due to conditions like Addison’s disease, hypothyroidism, or adrenal insufficiency can disrupt blood pressure regulation.
- Neurological Conditions: Disorders affecting the central nervous system, such as Parkinson’s disease or multiple system atrophy, can lead to orthostatic hypotension, where blood pressure drops upon standing up. People with such conditions feel the affects of Low BP especially after eating as more blood is used when digesting food.
- Nutritional Deficiencies: Inadequate intake of essential nutrients like vitamin B12 and folate can result in anemia, which can contribute to low blood pressure.
- Septic Shock: In severe cases of infection, the body’s response to toxins can cause a sudden and significant drop in blood pressure, leading to shock. Life-threatening allergic reactions (anaphylaxis) can also cause low blood pressure.
- Alcohol or recreational drugs: Recreational drugs and alcohol can cause hypotension for short periods of time.
- Extreme temperatures: Being too hot or too cold can affect blood pressure depending on your tolerance including your medical condition making the effects of high or low blood pressure worse.
Signs and Symptoms of Hypotension
The signs and symptoms of hypotension can vary depending on the underlying cause and severity of the condition. Common symptoms include:
- Dizziness or lightheadedness, especially upon standing up
- Fainting or syncope
- Fatigue
- Slow or fast heart rate
- Blurred vision
- Low cardiac output (how much blood your heart pumps).
- Low urine production
- Pallor
- Nausea
- Cold, clammy skin, cool kneecaps
- Rapid or shallow breathing
- Weakness
Diagnosis of Hypotension
Diagnosing hypotension involves a thorough medical history, physical examination, and various tests to identify the underlying cause and assess the severity of the condition. Hypotension itself is not hard to diagnose because you can even take your own blood pressure with a home device. Monitoring your symptoms over a period and at certain times of day can help you understand if you are suffering from hypotension. The real problem is figuring out why you have hypotension and if your health is in danger because of it.
Key diagnostic procedures may include:
Blood Pressure Measurement: Blood pressure is measured using a sphygmomanometer, with readings taken in different positions (lying down, sitting, and standing) to assess for orthostatic hypotension.
Blood Tests: Laboratory tests can help identify underlying conditions such as anemia, electrolyte imbalances, or endocrine disorders.
Electrocardiogram (ECG or EKG): This test records the heart’s electrical activity and can detect abnormalities indicative of heart problems.
Echocardiogram: An ultrasound of the heart that provides detailed images of its structure and function, helping to diagnose conditions such as heart failure or valve disorders.
Tilt Table Test: This specialized test is used to evaluate orthostatic hypotension by monitoring changes in heart rate and blood pressure while the patient is tilted at different angles on a table.
Treatment and Management of Low blood Pressure
Treatment of hypotension starts with diagnosing the reasons behind it. However, treatment becomes possible only when the issue causing it is treatable, in which case a doctor will recommend medication to manage the low blood pressure as symptom. In many cases, lifestyle modifications and conservative measures are sufficient to manage mild hypotension. However, more severe, or symptomatic cases may require medical intervention. Here are some common approaches to treating and managing hypotension:
Fluid Intake: Increasing fluid intake, especially water, can help raise blood volume and improve blood pressure. Avoiding excessive alcohol consumption is also important, as alcohol can contribute to dehydration and increase hypotension.
Increasing blood volume: Also known as fluid resuscitation, this requires administration of intravenous (IV) fluids or plasma or blood transfusions to raise your blood volume.
Salt supplementation: Consuming slightly more salt in the diet can help retain fluids and raise blood pressure, but this should be done under medical supervision, especially for individuals with certain health conditions like hypertension or kidney disease.
Compression stockings: Wearing compression stockings can help prevent blood from pooling in the legs and improve circulation, particularly in cases of orthostatic hypotension.
Medications: Depending on the underlying cause, medications may be prescribed to manage hypotension. These may include medication to increase sodium retention, to constrict blood vessels, or to address specific underlying conditions such as heart failure or adrenal insufficiency.
Lifestyle modifications: Engaging in regular physical activity, avoiding prolonged standing, or sitting, and gradually changing positions can help prevent orthostatic hypotension. Additionally, eating smaller, more frequent meals and avoiding heavy meals can prevent postprandial hypotension. Increasing your salt intake could also help increase blood pressure.
READ: Ways To Increase Your Low Blood Pressure
Identifying and treating symptoms: Identifying the signs of hypotension will help you understand what to do when it starts.
Treatment of underlying conditions: Addressing underlying medical conditions such as heart disease, endocrine disorders, or neurological conditions is crucial for managing hypotension effectively.
When is Hypotension an Emergency
- Low blood pressure becomes an emergency when you have:
- Have chest pain.
- Faint
- Fall due to dizziness or lightheadedness
- Symptoms of shock such as cold, sweatiness, rapid breathing, racing heart rate, blue tint in skin, lips, or fingernails.
Hypotension is a condition characterized by abnormally low blood pressure, which can have various causes and present with a range of symptoms. While mild hypotension may not always require treatment, more severe cases can lead to complications and warrant medical intervention. Early diagnosis and appropriate management are essential for preventing complications and improving quality of life for individuals with hypotension. If you experience symptoms of hypotension or have concerns about your blood pressure, it’s important to consult with a healthcare professional for evaluation and personalized management recommendations.